Program Implementation Process
Equitable Medicaid and Clinical Research operates through a clear, people-centered model that places underserved communities at the core of every activity. Our work begins with a simple question: what prevents individuals and families from receiving timely medical care where they live? From this starting point, we design practical systems that bring services closer to those who need them most, while supporting research that informs safer and more effective medical care.
Community engagement and trust-building
Our work starts at the community level. Before any medical outreach or research activity takes place, we engage local leaders, women’s groups, youth representatives, and health workers to understand existing gaps in care. These conversations help us learn about local health priorities, cultural norms, and practical barriers such as distance, cost, or lack of information. This process builds trust and allows communities to take part in shaping programs that respond to their real needs, rather than externally defined assumptions.
We place strong emphasis on listening, consent, and clear communication. Community members are informed about planned activities, their rights, and the services available to them. Feedback is encouraged at every stage, and concerns raised by community members guide adjustments in our work.
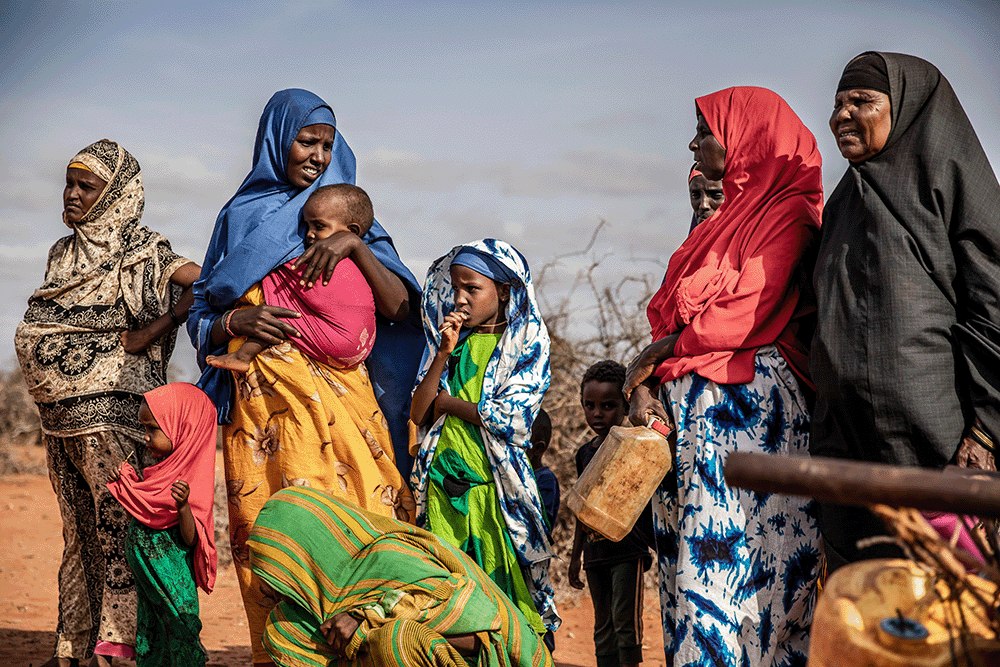
Service delivery in underserved settings
To reach rural and hard-to-access areas, we support mobile health services and community-based clinics that reduce travel burdens for patients. These services focus on primary healthcare, screening, health education, and referrals to higher levels of care when needed. Women, children, older persons, persons living with disabilities and low-income households are given priority, as these groups face the greatest barriers to care. Our activities are carried out within existing health structures to increase access while preserving local system capacity.
Use of digital tools
Technology supports our work by improving coordination, data collection, and follow-up. Simple digital tools are used to register patients, track services provided, and support referrals. In areas with limited infrastructure, we adapt tools to fit local realities, using offline systems where internet access is unreliable.
Digital records help reduce service gaps, limit duplication, and support continuity of care. They also allow us to analyze service data responsibly, while protecting patient privacy. This information supports planning, reporting, and learning across programs.
Clinical research and ethical standards
Clinical research is a central part of our work. We carry out studies that contribute to the development and evaluation of medicines, vaccines, and treatment methods relevant to populations that are often underrepresented in research. Our research activities follow strict ethical guidelines, with informed consent, participant safety, and data protection as core requirements. Research topics are selected based on public health needs and gaps identified through community engagement and health system data.
Capacity development
We invest in strengthening the skills of health workers, researchers, and community volunteers. Our training covers key areas of health practice, including clinical care, research ethics, data management, and patient communication. Strengthening local capacity supports continuity of services and reduces dependence on external personnel.
Women’s leadership is consistently promoted across our programs. As a woman-led organization, we encourage women to take on leadership roles in healthcare delivery, research coordination, and program management. This commitment supports balanced representation in decision-making and corresponds with the realities of many communities where women carry primary caregiving responsibilities.
Partnerships and coordination
Our work is carried out in cooperation with public institutions, health facilities, academic bodies, and development partners. These relationships allow shared learning, resource pooling, and coordinated service delivery. Clear roles and accountability structures guide all collaborations to maintain transparency and trust.
We also work with government agencies to support national health priorities and align activities with existing policies and standards. This coordination helps strengthen health systems rather than creating parallel structures.
Monitoring, learning, and accountability
Continuous learning guides how we work. Data from service delivery and research activities are reviewed regularly to identify gaps, successes, and lessons. Community feedback, staff reflections, and partner input all inform improvements in program design and delivery. Accountability to communities, partners, and supporters remains a core principle. We maintain clear records, provide regular updates, and share lessons learned. This openness helps sustain responsible growth of our programs.
Nuestros programas
Learn more about our programs and priority areas in various health sectors.
